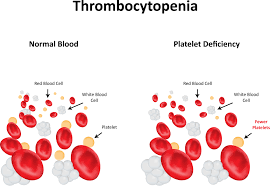
Thrombocytopenia is caused by several mechanisms. The two most common ones are decreased production in the bone marrow and increased destruction of platelets (immune thrombocytopenia purpura, drug induced, etc) in the peripheral blood. Thrombocytopenia due to dilution can occur in patients receiving multiple transfusions or in pregnant women as a result of increased plasma volume. Platelets are consumed in hypersplenism and disseminated intravascular coagulation. Pseudo or spurious thrombocytopenia is a relatively common cause of thrombocytopenia due to EDTArelated platelet clumping view image. Review of peripheral smear is diagnostic.
ETIOLOGY
HIV and Thrombocytopenia:
About 40% of HIV patients have some degree of thrombocytopenia. In 10% of patients, low platelet count may be the initial manifestation. Primary HIV associated thrombocytopenia is the most common cause, due to increased destruction and ineffective production of platelets. Primary HIV associated thrombocytopenia may also be indistinguishable from immune thrombocytopenia purpura. Some HIV positive patients may have splenomegaly with subsequent platelet sequestration.
Sepsis and Thrombocytopenia:
Thrombocytopenia occurs in up to 20-35% of patients admitted to intensive care unit. Sepsis is responsible for half of these. There are several mechanisms involved: bone marrow suppression, EDTA related platelet clumping (pseudo thrombocytopenia), immune and non-immune disseminated intravascular coagulation destruction/consumption of platelets. There is an inverse relationship between the severity of sepsis and the platelet count. Thrombocytopenia is an independent risk factor for mortality in patients with sepsis
Disseminated Intravascular Coagulation:
Disseminated intravascular coagulation results from injury to vascular endothelium, leading to exposure of tissue factor, which activates the extrinsic factor pathway in coagulation cascade. In this process, consumption of the coagulation factors and platelets leads to bleeding, hence the name consumptive coagulopathy. Several factors trigger disseminated intravascular coagulation, including sepsis, malignancy, extensive trauma/burns, intrauterine fetal death, etc. Prolonged prothrombin time and activated partial thromboplastin time, low fibrinogen, increased D-dimer, thrombocytopenia are all suggestive but not diagnostic. There is no specific treatment for disseminated intravascular coagulation other than addressing the underlying problem. Transfusion of blood products such as cryoprecipitate and platelets should be considered only if there is significant bleeding.
Thrombotic Thrombocytopenic Purpura:
This is a potentially life threatening entity which can be treated very effectively with total plasma exchange. Thrombotic thrombocytopenic purpura is thought to stem from deficiency of von Willibrand factor cleaving enzyme also known metaloprotease. It manifests as thrombocytopenia, microangiopathic hemolytic anemia (increased reticulocyte count, LDH, low haptoglobin and presence of fragmented red blood cells on blood smear), altered mental status, renal failure and fevers (the so called ‘pentad’). Unfortunately, there is no diagnostic test for thrombotic thrombocytopenic purpura. Presence of thrombocytopenia, microangiopathic hemolytic anemia with any of the aforementioned features is highly indicative of thrombotic thrombocytopenic purpura.
Immune Thrombocytopenic Purpura (TTP):
Immune thrombocytopenic purpura is usually idiopathic and occasionally may be secondary to an auto-immune process such as lupus, rheumatoid arthritis, or lymphoproliferative disorders (lymphomas or chronic lymphocytic leukemia). Infection with HIV, hepatitis B and C and helicobacter pylori may also be associated with immune thrombocytopenic purpura. Bleeding is rare despite severely low platelet count due to the presence of functional platelets.